Title: Prevalence and Impact of COVID -19 on In-hospital Outcomes and Associated Racial Disparities in Young Women of Reproductive Age Group (18-44 years) Hospitalized with Pulmonary Embolism in the US in 2020
Background:
Given the potential of thrombotic events such as pulmonary embolism in COVID-19, it is essential to comprehend the specific risks and effects on young women of reproductive age, a high-risk group for venous thromboembolism. There is a paucity of data regarding the prevalence and impact of COVID-19 in young women within the reproductive age group who were hospitalized with pulmonary embolism (PE) in the United States during the year 2020.
Methods:
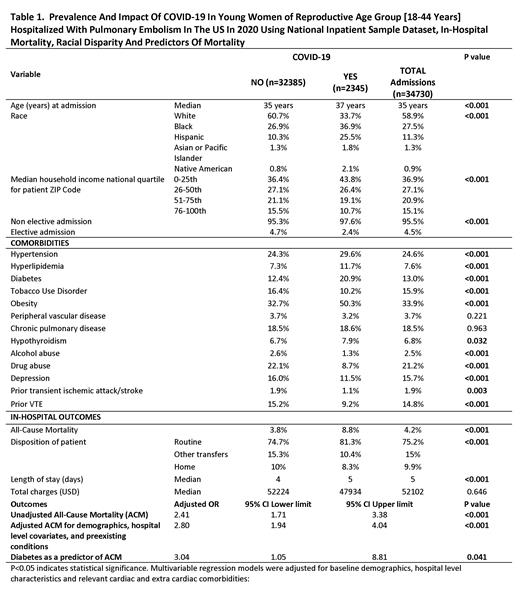
Utilizing the National Inpatient Sample (NIS) 2020 and relevant ICD-10-CM codes, we identified admissions for PE with COVID-19 vs. without COVID-19 among Young Women [18-44 years] hospitalized with PE. We compared the baseline characteristics and comorbidities between the two groups with and without COVID-19. Furthermore, we analyzed the multivariable adjusted odds ratio (OR) of all-cause mortality in COVID-19 with the non-COVID-19 cohort as a referent, subgroup odds for white vs. other races, and effect modification by diabetes mellitus (DM) as a comorbidity.
Results:
We identified 34,730 hospitalizations in young female patients of the reproductive age group (18 to 44 years) in 2020 with the diagnosis of PE, of which 2345 (6.8%) had COVID-19. The prevalence of PE was higher in COVID-19 cohort (1.6% vs. 0.6%, p<0.001). The majority of the patients with PE were Caucasian (58.9%) and in the lowest median income quartile (36.9%). Analysis of various comorbidities in both cohorts revealed a statistically significant higher prevalence of hypertension (29.6% in those with COVID-19 vs. 24.3% in those without COVID-19, p <0.001), Similarly, hyperlipidemia (11.7% vs. 7.3%, p <0.001), DM (20.9% vs. 12.4%, p <0.001), and obesity (50.3% vs. 32.7%, p <0.001), were more prevalent in COVID-19, indicating that patients who were admitted with PE with concomitant COVID-19 were of poorer overall cardiovascular health than those with COVID-19. Unadjusted all-cause mortality odds ratio was 2.41 (1.71-3.38, p <0.001) in PE with COVID-19 than non-COVID-19. Adjusted all-cause mortality for demographics, hospital level covariates, and pre-existing conditions revealed similar statistically significant findings, with the odds ratio being 2.8 (1.94-4.04, p <0.001). There was no racial disparity observed in all-cause mortality for non-whites compared to white patients admitted with PE and COVID-19 (p=0.064). Furthermore, all-cause mortality in patients with COVID-19 and PE was found to have an odds ratio of 3.04 (1.05-8.81, p=0.041) in a subset of DM compared to non-DM. The results have confirmed a further robust positive association with increasing mortality risk with DM in young women hospitalized with PE and COVID-19.
Conclusion and Relevance:
There was a nearly three times higher prevalence of PE and 2.5 times higher odds of mortality in Young Women of Reproductive age [18-44 years] hospitalized with PE with COVID-19 as compared to without COVID-19. The effect of PE and a higher risk of mortality are already established with COVID-19; however, there is a paucity of data in young women, which warrants more prospective studies to evaluate the long-term thromboembolic risks of PE and associated events in this population. The findings of this research could have significant implications for understanding the relationship between COVID-19 and PE in this patient population. Special emphasis needs to be laid on improved healthcare strategies, targeted interventions, and patient education in this cohort to establish future research agendas and provide better health care outcomes for this vulnerable group with established risk factors like diabetes.
Key Words: COVID-19, Young Women, Pulmonary Embolism, In-Hospital Mortality, Racial Disparity, Predictors of Mortality, Diabetes Mellitus, National Inpatient Sample
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal